I’ve been a Chiropractor and a Pediatric specialist for over 16 years. I’ve had the joy of caring for thousands of pregnant women and helping them to have safer, easier births. I’ve also had the honor to care for their babies, either as preventative wellness care, or to address issues such as poor breastfeeding practices, colic, or a myriad of other imbalances. This led me down a path of higher education to learn more about the causes of these issues; finding an absolute fascination with the cranial/sacral system and all of the infinite connections. As I immersed myself in the birth world and networked with doctors, midwives, lactation consultants, doulas, etc.… hoping to gain referrals to help these little ones, I eventually realized that there are some huge barriers preventing the ideal collaboration of care.
Let’s step back for a moment and set the stage.
This is a very common scenario in my office – New parents bring their precious newborn to my office for a consultation. They are TIRED. Not only did the birthing parent just endure a long and (often) difficult birth process along with all of the hormonal changes occurring in their body, they are also not sleeping much at all due to the demands of their child. Often there are other young children at home as well needing attention.
Their newborn is fussy, inconsolable, and not breastfeeding well. If the baby is able to achieve a strong latch at the breast, it is often extremely painful for the parent causing cracking and bleeding of the nipples. Perhaps the baby cannot latch well, he/she is then not able to drain the breast during feedings, resulting in engorged and painful breasts, or even worse- mastitis. Perhaps the baby was premature or had other difficulties at birth. Perhaps there is a concern that he/she is “failing to thrive” and has not gained enough weight.

The parent might be “triple feeding” which means that they are breastfeeding AND pumping excess breastmilk to give to their baby in a bottle later. This takes ALL of their time and energy to feed around the clock. Perhaps they have all but given up nursing at the breast and are resigned to pump and bottle feed- again, taking extra time and not receiving the normal rewards of bonding and physical attachment. They are at their emotional and physical wit’s end and have nowhere else to turn. They often show up at my office after exhausting the available support from the hospital staff.
This parent likely delivered her baby in a hospital or birthing center where she was visited by a Lactation Consultant before going home with her baby. The lactation consultant probably spent a short amount of time helping the parent with breastfeeding practices such as ways of opening the baby’s mouth wider, placing the nipple deeply in its mouth, holding her baby in more comfortable positions, etc. If the baby struggles to attain a deep, strong latch, there is often no more advice than, “Keep trying”. Once the baby is at home, if nursing continues to be a struggle, then the parent often returns to the hospital lactation consultant for another short consult. Here, the baby is usually weighed to see if he/she is gaining a normal amount of weight and if they are transferring milk. If not, then often formula is introduced. This can lead to a spiral of low milk production by the parent and often fails to establish normal breastfeeding practices. Once again, if the baby is not able to do these things, there is usually little instruction about addressing the physical limitations of the baby.
Let’s address WHY the baby might be struggling first, and then we’ll address WHY the Lactation Consultant is all too often unable to help with this scenario.
In a nutshell:
When breastfeeding challenges occur, oftentimes the problem is not with the mother’s technique, but rather with the baby himself – barriers within the alignment and tone of his body causing abnormal function and preventing normal breastfeeding practices.
The most common physical barriers preventing the baby from breastfeeding normally are:
Misalignment of the cranial bones and spine
The skull (also called the cranium) is made up of 8 cranial bones and 14 facial bones which support the brain, eyes, inner ear and Eustachian tubes. They form the sinuses, the palate, and the jaw (Temporo-mandibular joint or TMJ). The normal alignment of the jaw and palate are crucial to allow the normal movement of the jaw, the ability to latch properly, and the ability for the tongue to reach the roof of the mouth for a proper seal.
The normal alignment of the upper neck is necessary to allow the baby to turn its head properly during breastfeeding practices. Even the alignment of the baby’s lower pelvis (sacrum) determines the tone of his body (tense and uncomfortable or relaxed). The bony structure also is the attachment site of all of the muscles necessary for the baby to breastfeed at well, from the direct muscles of the tongue to the accessory muscles of the jaw, neck, and pharynx.
Cranial Nerve Impairment and Breastfeeding Practices
Cranial Nerves originate in the brain and exit the skull through small openings called foramen. There are four cranial nerves which allow for the main actions of breastfeeding:
- Hypoglossal (CN XII)- Innervates all but one of the extrinsic and intrinsic muscles of the tongue. It originates in the Medulla (brain stem). The medulla is surrounded by the Foramen Magnon of the Occiput (base of the skull) and is affected by the alignment of the Atlas (first cervical vertebra). It exits the skull through the Hypoglossal Canal, a small opening between the Occiput and the Atlas, and branches of it pass through the cervical spine before traveling to the tongue.
- Glossopharyngeal (CN IX)- Innervates mainly the Stylopharyngeus muscle of the larynx which allows for the action of swallowing. This cranial nerve originates in the Medulla of the brainstem and exits the cranium through the Jugular Foramen (along with the Vagus N). Upon exiting the skull, the motor fibers of this nerve descend deep to the Styloid Process of the Temporal bone and wrap around the posterior border of the stylopharyngeus muscle.
- Accessory (CN XI)- Mainly innervates the SCM (Sternocleidomastoid Muscle) and the Trapezius, which also play a role in swallowing. This nerve also shares the Jugular Foramen with CN XII and CN X.
- Vagus (CN X)- This is, without a doubt, the KING of the cranial nerves. It originates from the medulla of the brainstem. It also exits the cranium via the Jugular Foramen, with the Glossopharyngeal and Accessory nerves respectively. It has the longest pathway of any other nerve in the body. It transmits information to/from the brain to tissues & organs elsewhere in the body. It communicates between the brain and the gut. It balances the heart rate and blood pressure, allows for relaxation with deep breathing, coordinates the inflammation process, plays a key role in anxiety management, and many more things. It also innervates the other intrinsic muscle of the tongue- the Palatoglossus. If this nerve is compromised, it not only impedes the swallowing reflex but also leads to an overall unresponsive or overstimulated baby. This presents itself as colic, reflux, excess gas, or a combination of symptoms labeled as “Failure to thrive”.
*** Any misalignment of the cranial bones which form the foramen can cause pathological irritation of these cranial nerves and impede their function. Notice that ¾ of these crucial nerves pass through the Jugular Foramen, formed by the union of the Temporal Bones and the Occiput. This is a very common area of misalignment in the newborn skull which has a very direct impact on the strength of the tongue and the baby’s ability to swallow.
Imbalance in the Cerebral-Spinal System
The cranial bones also support a system of fibrous folds inside of the skull which forms channels or ducts through which the cerebral spinal fluid flows. This fibrous tissue begins inside of the skull as the periosteum (or lining of the interior of the skull) and continues all the way down the spine to the bottom of the sacrum. This spinal fluid (CSF) flows up and down inside of the spinal column and cranium by a pumping mechanism created by the motion of the sacrum and the cranial bones. In the adult, this motion is accomplished by the simple act of walking.
In the newborn, this motion is established during the birth process as the baby is being squeezed through the birth canal. This does not occur in the event of a Cesarian Section birth. The CSF fluid controls the temperature in the cranial vault (like anti-freeze). Increased temperature leads to a tendency for seizure activity. The CSF fluid also provides nutrition and waste removal to nervous tissue and acts as a protective barrier (chemical and physical) for the brain and spinal cord. Any misalignment of the cranial bones or the spinal/pelvic segments can cause an imbalance of the normal pressure of this fluid and translates to the over-stimulation of the baby’s nervous system. The converse is also true- if the CSF pressure is unbalanced (perhaps due to a C-section birth or other trauma) then the cranial bones can become pulled and misaligned.
Phew! OK. That was a big stage to set! You can see clearly that there is A LOT going on within the newborn’s body that dictates if he has the ability to breastfeed normally. Now… why isn’t that all talked about in the hospital by the Lactation Consultant?
One barrier is we do not have a collective understanding of each other’s discipline. The OB or Nurse Midwife probably doesn’t know that a Chiropractor can address imbalances of the baby’s jaw for a better latch and suck. The Lactation Consultant may identify that there is a structural issue with the baby preventing him from nursing properly, but she may not have the anatomical knowledge to identify it. *** This is, in no way, meant to suggest that Lactation Consultants are not highly knowledgeable and skilled caregivers. I have a huge amount of respect for these amazing professionals. We just all have different educational backgrounds and scopes of practice.
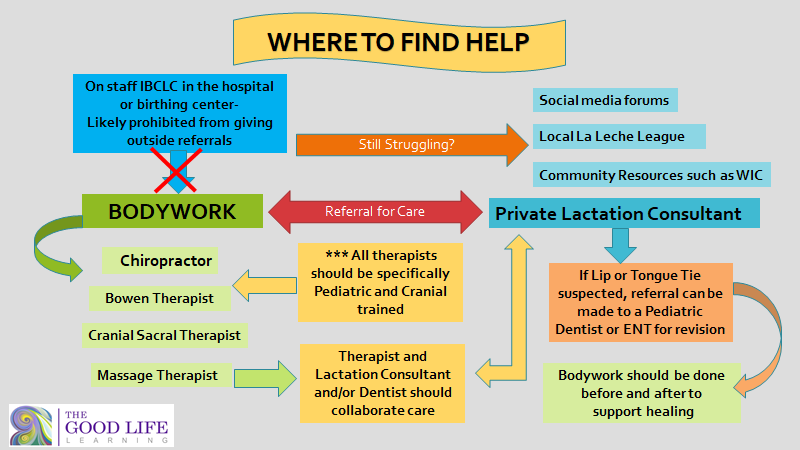
Another very unfortunate and huge barrier is that, even if the birth professional identifies the issue AND knows that bodywork can help to correct it, their hands are all too often tied to say anything about it to the parent due to hospital liability policies and administrative restrictions. Many of my close associates and friends are wonderful, highly skilled Lactation Consultants who work in the hospital setting. They recognize and acknowledge all of the information that I’ve presented here about the baby’s condition but tell me that they are expressly forbidden by their administrators to refer the baby out for care to a chiropractor, cranial therapist, etc.… One such friend of mine recently even told me that they are no longer allowed to mention the existence of a tongue-tie (that is a whole different article).
WHY does this limitation and lack of referrals exist? Well- Let’s be honest. One reason is that there simply is not a continuity of care among all Chiropractors and Bodyworkers. WHO do the medical professionals confidently refer these babies to? Not every chiropractor is the same. This is a key point. Like it or not, we have to recognize that not all Chiropractors or bodyworkers (even those who are pediatric trained in general) have the further training to do specific cranial work. It often frustrates me when a birth professional or dentist says, “ I refer my patients to the chiropractor down the street” when that person very likely is not trained appropriately or doing what is truly needed for that baby. And then, guess what? If there is not a corrective outcome, everyone thinks that the care was not effective. It just was not the appropriate care. It’s like hiring a house painter to restore the Sistine Chapel. The tools are the same, but the Pope just is not going to be happy with the result. The only way that these children are going to receive the care that they need is for Pediatric Chiropractors to become skilled in the specialty of specific cranial work through continued education.
Another reason is that Evidence-Based research of the effectiveness of this care isn’t widely circulated. Fortunately, there is more validating research being done now. The ICPA offers a feast of amazing Evidence-Based research. This research won’t reach the medical professionals, though, if we chiropractors don’t step forward in our communities and share it. It’s sad, but true… We Chiropractors often do not have the confidence of other medical professionals so that we may apply our skills.
Where will that parent find the needed support if no information is given soon after birth? The sad truth is that, if the proper support is not given- from the Lactation Consultant, Chiropractor or cranial specialist, ENT or DDS, etc… the parent will resort to feeding their baby formula. Studies show that if successful breastfeeding practices aren’t established within 2 weeks of birth, parents usually give up. It is the responsibility of the Chiropractic profession to advance our skills in specific cranial therapy and to share our knowledge and research in our communities.
The physical, neurological, and emotional benefits of breastfeeding practices are undeniable. Breastfeeding provides children with lifelong protection against many diseases and exposure to toxins. This is a clear way to support the well-being of our children in a world where they are so open to negative exposure. The physical limitations of the baby often make it so difficult to perform breastfeeding practices, that the parent gives up. It’s SO sad when help was there, but nobody made the referral!
My driving passion is to bridge that gap- to train skilled therapists of all disciplines and to complete the circle of care. It’s SO worth it.
To learn more about breastfeeding and the anatomy involved in infants and how it affects breastfeeding, real-life case studies with breastfeeding patients, a host of interviews with lactation consultants, diagrams, demonstrations, and visual examples to teach the global subluxation pattern – The Anatomy of Breastfeeding. This new, updated, accredited continuing education course is for Chiropractors who are looking to improve their careers, learn from leaders and experts in their industry, and looking for new opportunities! The course is approved for 10 chiropractic CE hours.

